Conditions I treat......... Circular Frame Treatment: Lengthening & Deformity Correction
Circular frames
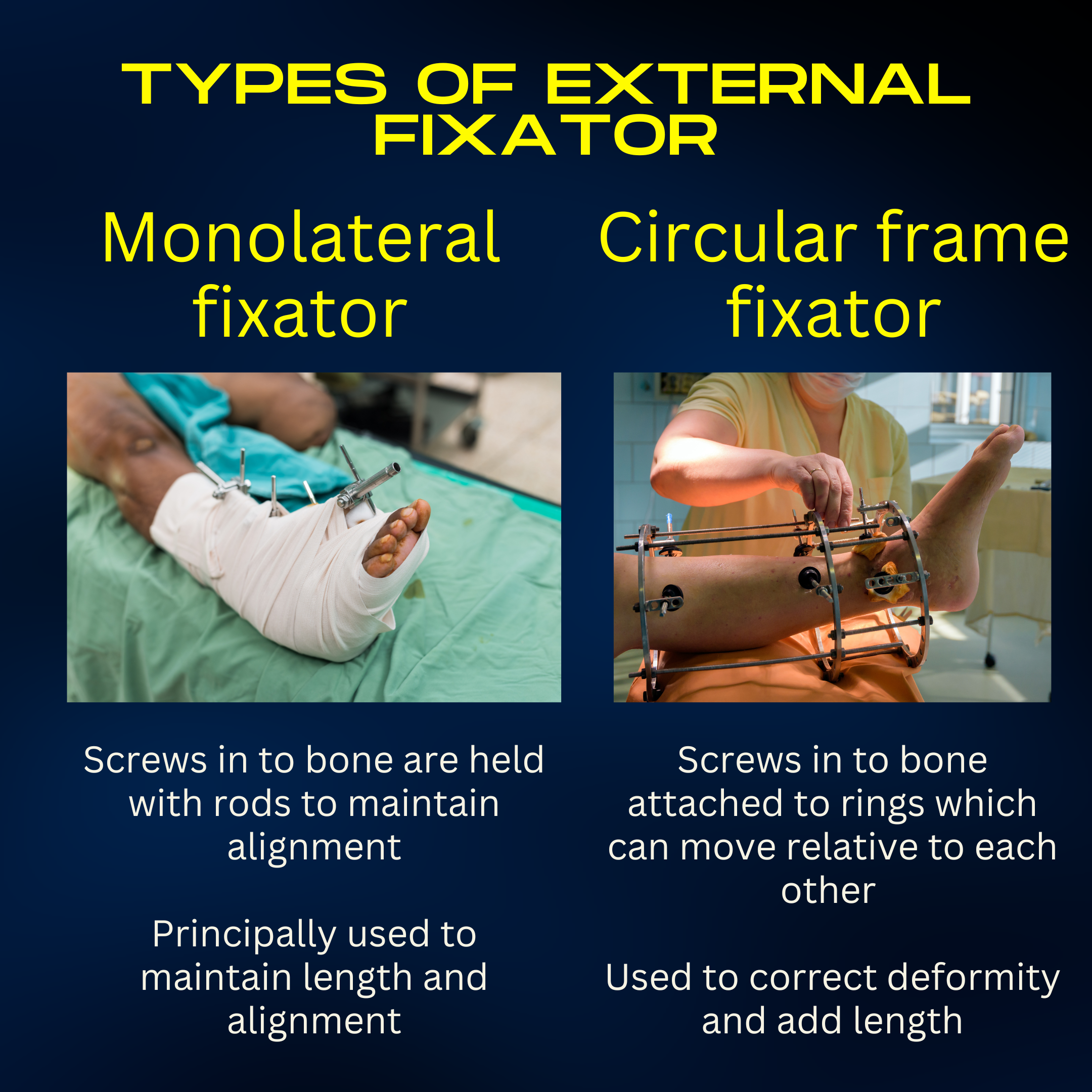
Limb reconstruction is a very distinct speciality focussed on restoring normal anatomy by correcting deformity and length in the limbs. It has evolved into a separate art distinct from the rest of orthopaedics principally because of the implants that are frequently employed to achieve this - circular frame external fixators. Whereas simple external fixators which work in one plane (mon-lateral fixators) are often used to hold alignment wilst planning more definitive surgery, circular external fixators are capable of achieving so much more....
Ilizarov introduced the world of Orthopedics to circular frame external fixators and Orthopaedics was forever changed. These revolutionary devices didn't just correct deformities in bone. They enabled a surgically divided bone to be lengthened by several centimeters in a predictable and reproducible fashion. Despite this seismic leap in what orthopedic surgery could achieve, this technology has, to some extent, remained a slightly arcane art. It is practiced by only a small minority of Orthopedic Surgeons. Circular frame constructs and their application are completely unlike any other type of orthopedic surgery and consequently, more challenging to grasp and master. Often in other orthopedic surgery (sadly), planning is, at best, seen as optional and, at worse, forgotten altogether. However in circular frame surgery it is mandatory. Calibrated x-rays, rulers, protractors, simulated corrections by cutting up an image of a bone and then piecing it back together all consume time and intellectual resources even before a patient comes close to the OR. The surgery is usually long and, to the casual onlooker, a tad difficult to fathom. Wires and bone screws are inserted under x-ray guidance without ever physically seeing the bone. Painstakingly but methodically a circular frame is constructed around the limb. Even the division of the bone is a "low energy" affair undertaken without power tools. Multiple drill holes are made at the intended level and then connected through a small incision with an osteotome (fancy chisel). Manual dexterity counts for little as complex judgements are teased out in the Surgeons mind whilst the physical reality of what the surgeon appears to be doing seems actually quite dry.
For all these reasons and more, circular frames will always remain a niche practice within Orthopedics. Fraught with complexity, lacking the drama of conventional open surgery and engendering long treatment programs that don't yield instant results are major factors that put off surgeons from this branch of Orthopedics. To add to the woes, circular frames are the MOST patient intrusive device in Orthopedics. Having a cage attached to your leg for several months with frequent hospital visits for adjustments requires patients to be appropriately counselled before and throughout treatment. In fairness, counselling patients through long treatment programs is not high up on the list of why doctors choose to be Orthopedic Surgeons.
So why do I and others undertake this surgery. For me at least, there is a very simple answer-
"In deformity correction and lengthening, a circular frame is the logical choice when........ a circular frame is the only reasonable choice." Assad Qureshi
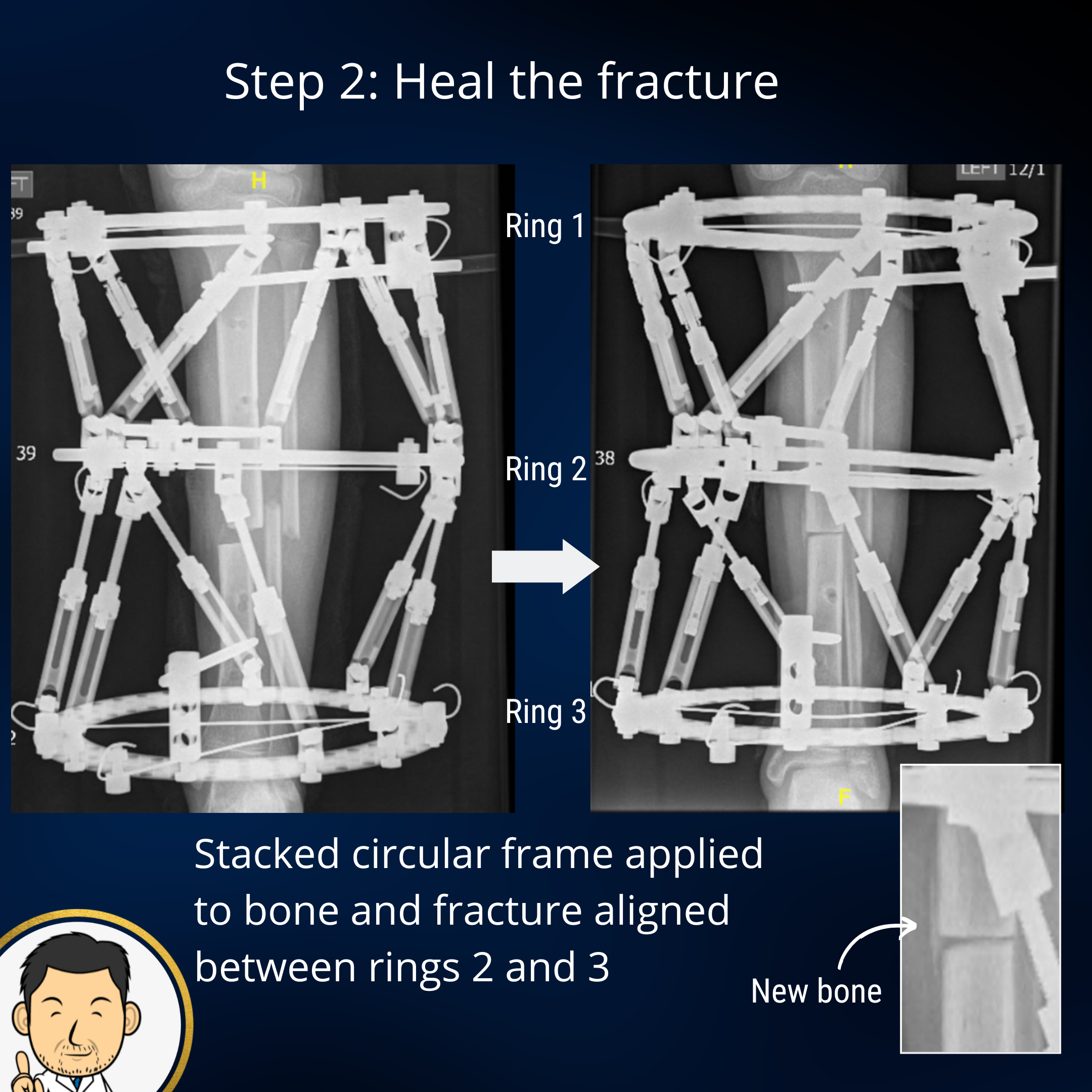
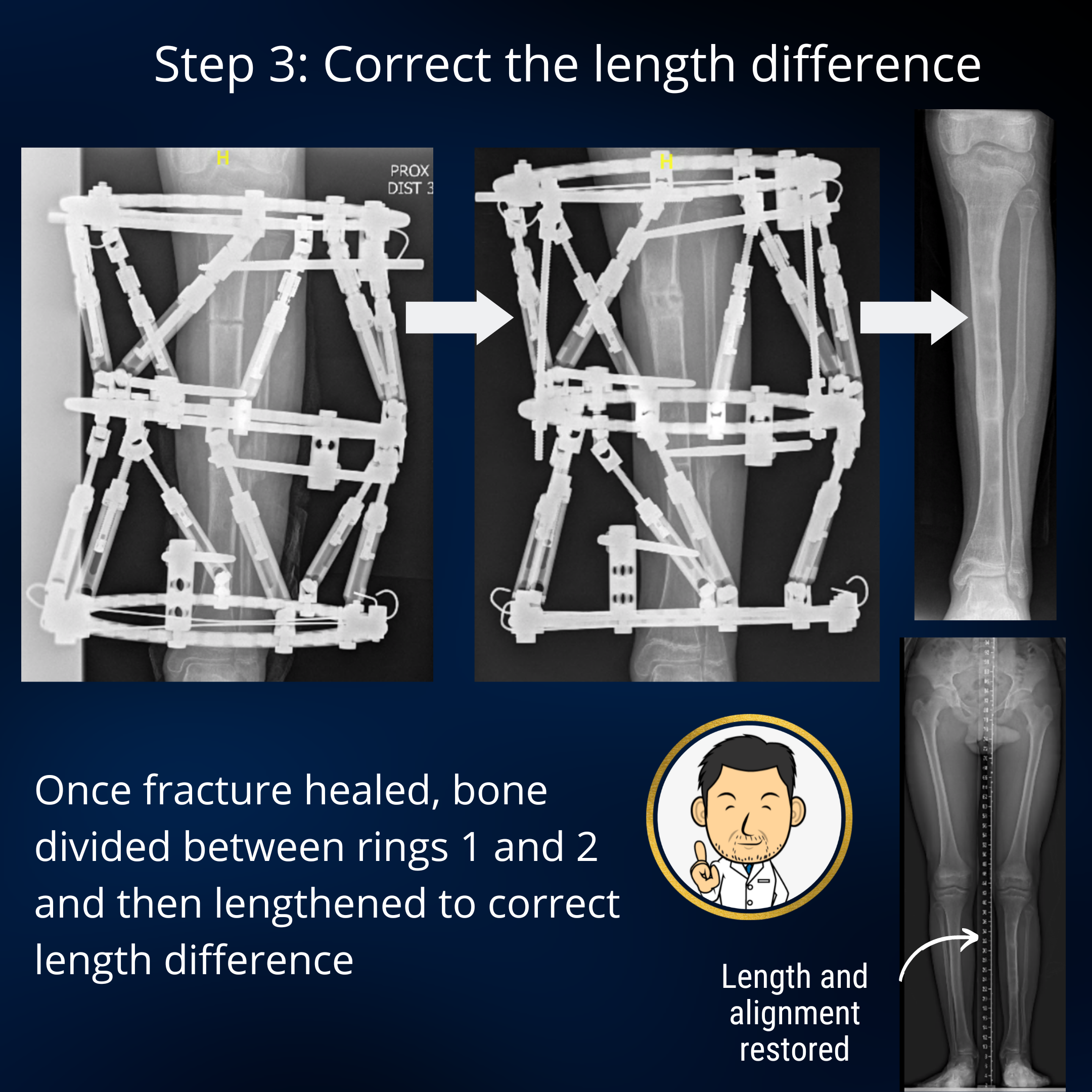
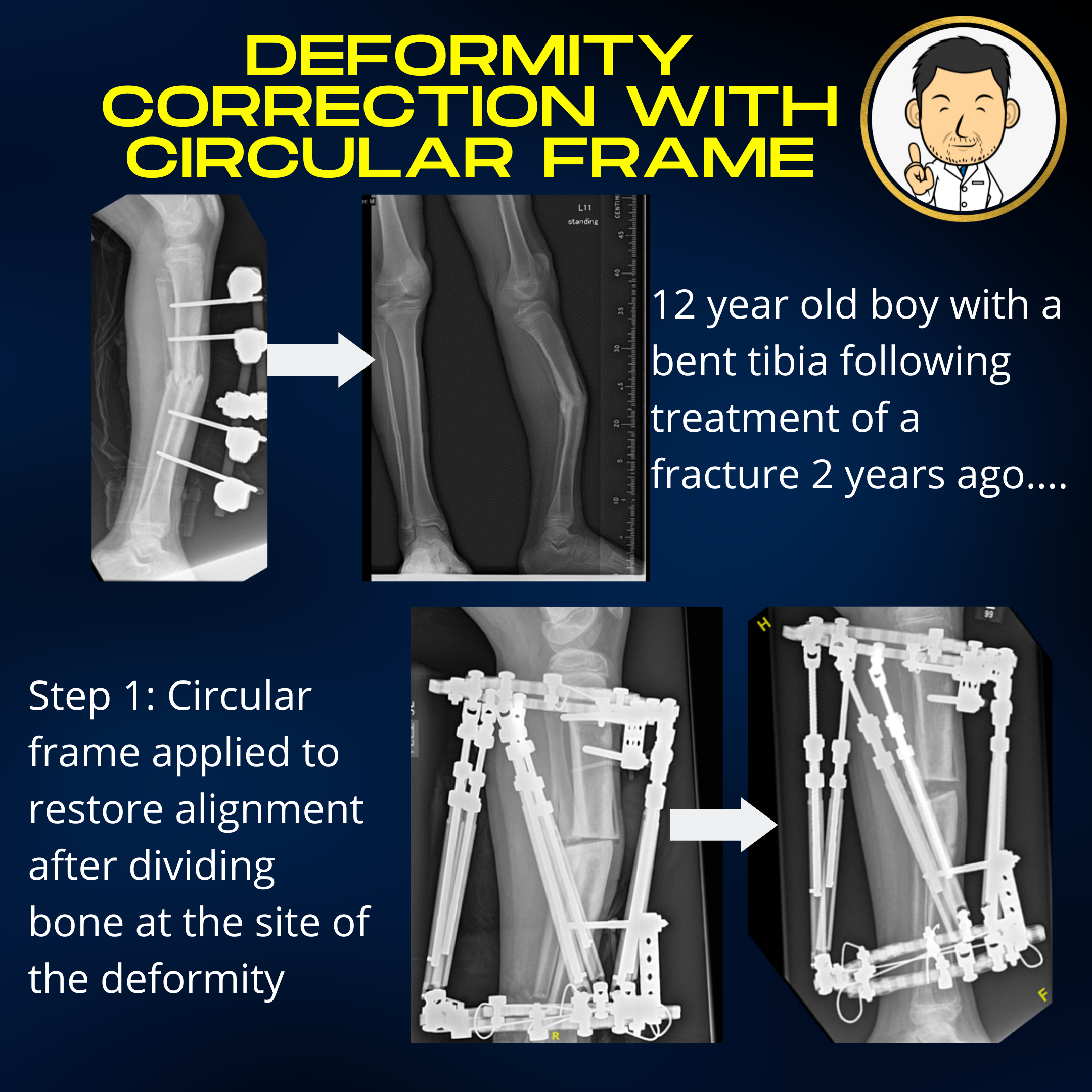
Circular frames came into being precisely because they were able to achieve a successful outcome in specific orthopedic conditions that could not be achieved by any other means. Predictable and reproducible lengthening, fracture healing in the presence of deep infection, bone transport for bone loss...up until a few decades ago, all very difficult to achieve a successful outcome without using a circular frame. Let's take a look at a case to get an idea of how it all works...
Types of circular frame
Without delving into technical specifics at a level of abstraction where everyone (myself included) stops reading this page beyond this sentence, there are two basic types of frames:
- Ilizarov circular frames - Rings are anchored to bone with wires predominantly. The rings are moved apart to correct deformity and lengthen the limb by adjusting the lengths of connecting rods. Introduction of plates and hinges allows correction of rotation and angulation. Treatment programs are designed by the Surgeon who looks at all the moving parts in the construct and decides the sequence and magnitude of manual corrections. A surgeon can look at the construct design in terms of where the rods are connected and the hinges are placed, and be able to work out what correction is occurring.
- Hexapod circular frames - Rings are anchored to bone with wires and bone screws. A pair of rings are connected by 6 struts with adjustable length. Varying the lengths of individual struts allows the two rings to adopt (almost) any orientation in 3d space relative to each other. Treatment programs are designed with the aid of computer programs. Dedicated software maps the frame to the bone. Inputting the deformity characteristics and desired correction, enables the software to come up with a list of daily strut adjustments which will achieve this. A surgeon looking at this construct alone can't deduce the vector of deformity correction unlike an ilizarov frame. Perhaps the most unsettling aspect for a surgeon - you have to trust a computer program to achieve the desired alignment.
There are many Ilizarov purists in the world and indeed heaxpods owe a debt to Ilizarov having inherited his guiding principles. However, I prefer hexapod constructs for the sincere reason that they are a lot easier to devise and apply for complex deformities. They also allow an infinite number of course re-directions during treatment to fine tune the correction and achieve alignment and length as close to perfect as possible. However, I do use Iliazrov principles when applying my rings to make my construct closely aligned to the bone's intended correction. A fully corrected frame aligned with the mechanical axis of the bone has optimal mechanical properties for load transfer and bone healing.
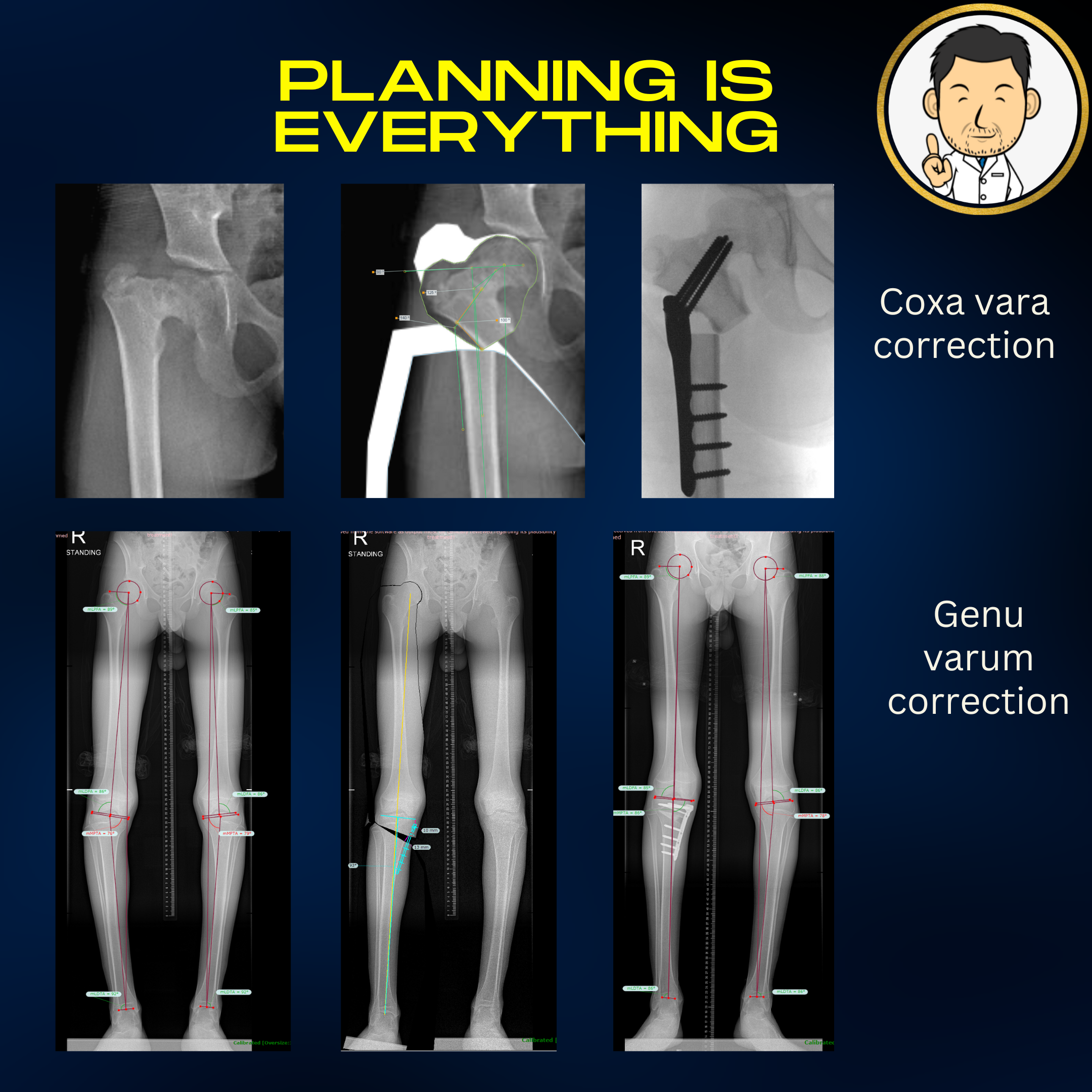
Deformity analysis and planning
There may be instances where we are only lengthening or only correcting a deformity. However, more often than not, we need to do both - lengthen and correct angulation. Planning is essential to determine where we need to break the bone and what we want the final result to look like in terms of alignment and length. Software programs such as Click2correct and Traumacad have largely supplanted drawing lines on printed x-rays. These software programs allow us to undertake the deformity analysis - measure the length of the limbs and individual segments, define the mechanical axis of the limb and assess the the plane of the knee and ankle joints relative to the ground. However, they also allow us to simulate the correction to ensure that the intended surgery will normalise all of these parameters. As much as I enjoy the surgery, I really enjoy the planning.
The frame journey
Usually I have quite a few patient consultations before embarking on frame treatment unless it is a trauma scenario. The purpose is to tailor patient and parent expectation regarding treatment. Frames are intrusive and "attached to the patient" for a very long time - months rather than weeks. They also need to be looked after. Parents have to appreciate that they will need to do strut adjustments during lengthening. Motivation is crucial - although uncomfortable at first the child will need to walk with the frame and engage with physiotherapy to prevent muscle tightness developing with lengthening. Once everyone is engaged and ready, it's on to surgery.....
I usually build the frame in theatre on the patient (there are some who pre-build the frame before the surgery, sterilise and then put it on in theatre). The frame is connected to the limb by a combination of bone screws and wires. Once the frame is connected the bone is divided in the appropriate location with the frame in situ. Depending on the frame construct, surgery can take a few hours. As the Resident, a double espresso is advisable. In a literal sense the surgery may be "riveting" but almost never in a metaphorical sense (the fact that you never see circular frame surgery in medical dramas lends some insight into how cinematic those few hours can be).
A latency phase of one week allows the crucial blood clot to form at the site of bone division (the precursor to the fibrous tissue and eventual bone which will form in the gap). The lengthening and/or correction is then undertaken with daily 1mm incremental distraction of the frame. This is the crucial rate for bone formation in the gap - go faster and you risk poor bone formation (regenerate) in the gap. Go slower and the bone may prematurely unite and cease lengthening. At a rate of 1mm/day, a 5cm lengthening will take 50 or so days. During lengthening, physiotherapy is crucial to maintain flexibility of the joints and prevent contractures because the muscles will tighten as the bone is drawn out to the intended length.
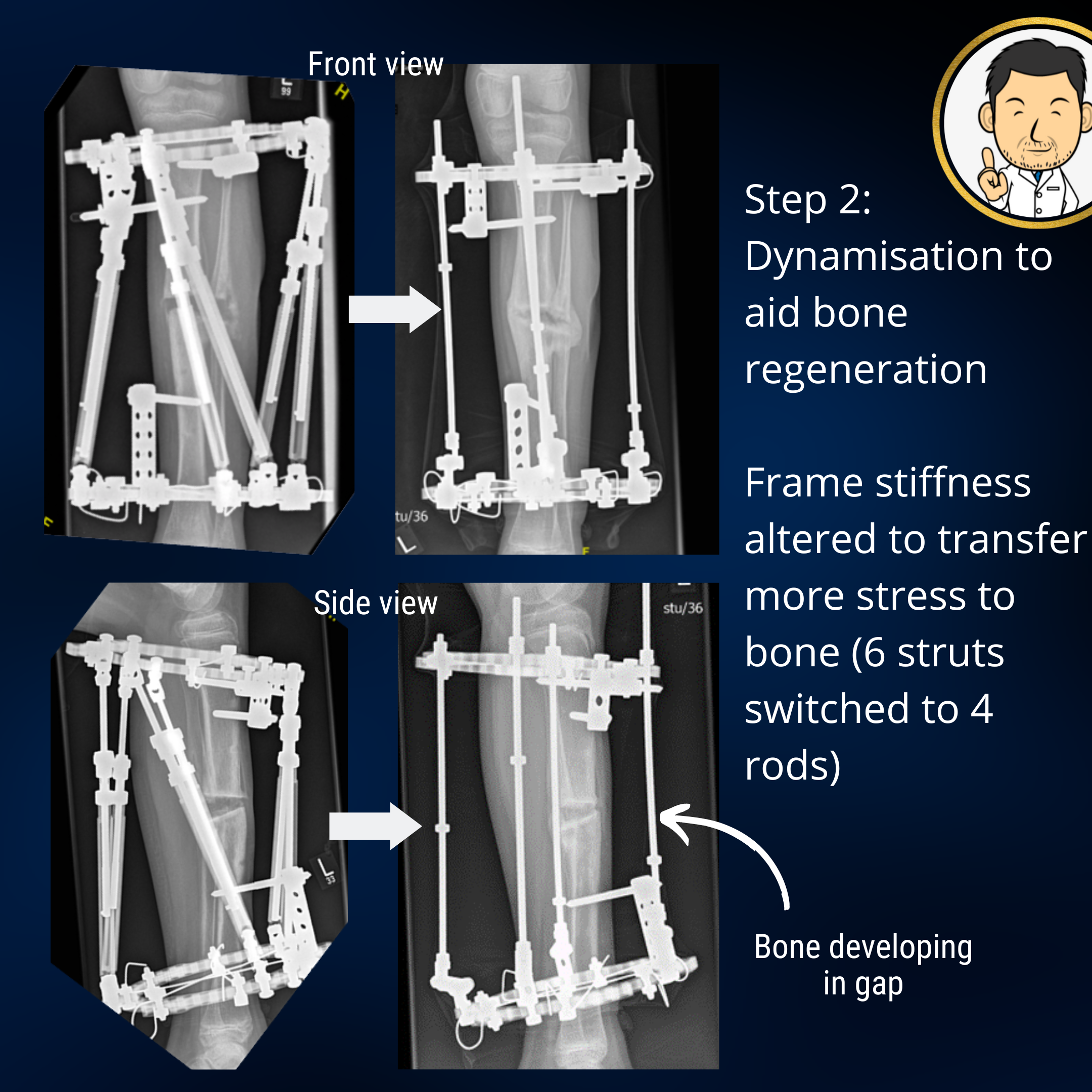
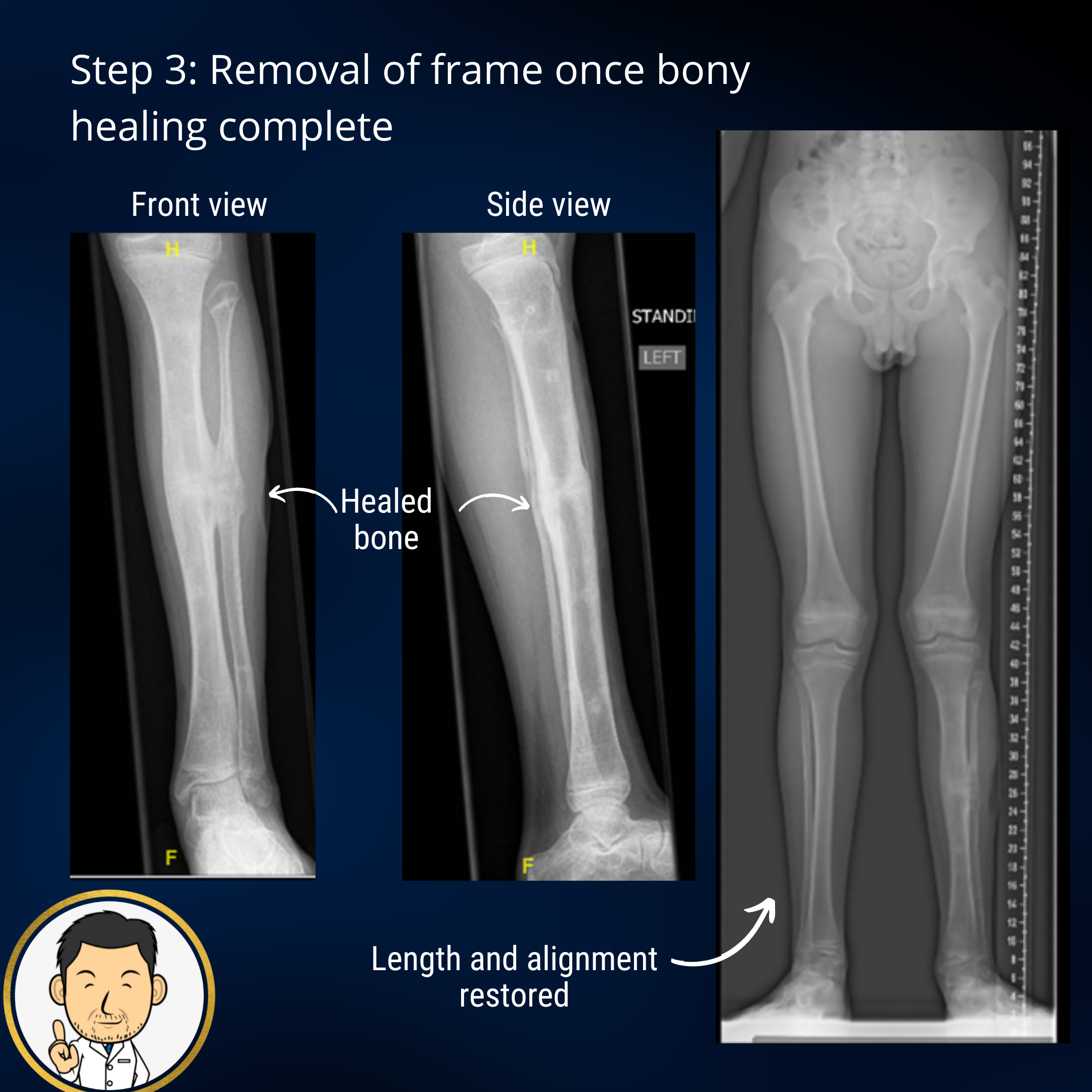
Once the lengthening is complete, the consolidation phase begins. This is where we await the maturation of the new bone in the formed gap to become strong enough to be able to remove the frame. This usually lasts for several months. I am a keen proponent for removing the frame as early as possible. However if the frame is removed too soon, fracture may occur through the bone regenerate......and it's back to square one (well not quite but it does mean more treatment time in a frame or plaster). Strategies I employ to hasten removal of the frame include:
- Physiotherapy to encourage (and ensure) weightbearing - loading the limb transfers mechanical force to the bone regenerate hastening its maturation. When I see a child not walking on their frame during the consolidation phase, I get worried.......
- Dynamization - Labour intensive but worth it. Tinkering and adjusting the frame construct to make it lighter and more flexible transfers greater stress to the bone regenerate. Adapting the frame to enable a millimeter or two of telescoping for compression is another technique. Sequentially employing these techniques at weekly clinic visits and instructing patients how to do them at home is classic Ilizarov teaching on bringing your "A" game to play.
- Cast brace immobilisation after frame removal - If the bone regenerate is almost there, rather than risk fracture leaving the limb free after frame removal I usually apply a cast brace. A cast brace is a plaster cast around the thigh and below the knee connected by adjustable hinges (admittedly does make a patient look a bit like Robocop from the 80s). The plaster cast provides protection and the hinge restriction ensures that deep bending of the knee (which imparts a very large bending moment on the bone) is avoided. Compression of bone regenerate is good, bending is bad. Six weeks in the cast brace is usually sufficient to effect the final stages of bone maturation.
The patient journey is long but good communication, frequent visits during the more involved parts of treatment, physiotherapy support and involvement of clinical psychologists all help to produce a good clinical outcome.